Doing the Right Thing
Dr. Stephen H. Tsang
The headline on the Columbia University web site reads "With Cells from Patients, Researchers Recreate Eye Disease in a Dish." The story goes on to describe a game-changing breakthrough that paves the way for the personalized treatment of age-related macular degeneration (AMD). Skin cells, taken from patients whose genes increase their risk of developing AMD, are converted into pluripotent stem cells, then prompted to become retina cells and "aged" to mimic the diseased retinal cells of a 60-year-old. These are the first "living" human cells in which treatments for specific AMD patients can be tested.
Listed among the sources of support for the study are the following: unrestricted department funds from Research to Prevent Blindness (RPB), the RPB Physician-Scientist Award, and the RPB Medical Student Eye Research Fellowship. This story starts with a RPB Medical Student Fellowship, but not the one cited in the study.
"I have been both the recipient of, and a mentor for, an RPB Medical Student Fellowship," says the first author on the paper, Stephen H. Tsang, MD, PhD, Columbia University College of Physicians & Surgeons. Dr. Tsang is an internationally recognized physician and geneticist specializing in the treatment of retinal degenerations. His recent mentee is Huy Nguyen, the recipient of the RPB Medical Student Fellowship cited in the paper, who will be starting his residency in ophthalmology at Massachusetts Eye and Ear Infirmary (MEEI).
Ever since Dr. Tsang's own experience as an RPB mentee, he has sought to help PhD students and postdoctoral fellows develop their full potential to become outstanding scientists, keeping an open-door policy with students. "In both roles," says Tsang, "it has been apparent that RPB seeks to have the highest impact, allowing scientists to pursue out-of-the-box thinking as it evolves. An RPB grant is not like a conventional grant, which typically can only be applied to work that is defined within a proposal.
"As an RPB Medical Student Fellow, you are required to work with a mentor. My mentor was a well-known molecular virologist and cancer biologist. But he didn't have the flexibility to fund work outside of his grant project. If I wanted to test my own hypothesis in his lab, I would have to find research money to fund my project. For this, there's no other mechanism than the RPB Medical Student Fellowship. Some of my work from that Fellowship ended up being published in Science. The rest of the results eventually ended up in a Journal of Neuroscience paper that I worked on as a resident."
He laughs: "In fact, even as a resident, RPB sustained me. There was an additional award mechanism that I received from RPB: the RPB/Association of University Professors of Ophthalmology (AUPO) Resident Award. It does not provide financial support, but early in your career it creates recognition for your work among colleagues because you are invited to make a presentation to chairs of departments of ophthalmology and directors of research.
"This kind of support is critical because, during residency, there's a tendency to constantly question whether or not you're making the right choice by going into research. This mentality is not surprising given that as a resident you can be praised by cataract patients as 'having the hands of god' after restoring their vision, while returning to the lab to face humbling, discouraging and sometimes even scathing comments from grant and journal reviewers. It is understandable that a high number of residents go into private practice as opposed to academic ophthalmology.
The encouragement from RPB that I received at the beginning of my research career was a crucial endorsement that I was doing the right thing.
"Eventually, after I became both a clinician and a researcher, RPB supported me in that decision as well. In 2005 I received the RPB/Becker/AUPO Award, which was designed to strengthen the role of the physician-scientist in ophthalmology. That award was essential in generating preliminary data for my NIH funding.
"In my RPB projects and beyond, I have always sought to combine the expertise I have acquired as a researcher with clinical experience to advance the cutting edge of gene therapy and regenerative medicine. I believe that collaboration and knowledge sharing are vital components of today's research endeavors. With government support, grants from other sources and ongoing support from the RPB Unrestricted Grant at Columbia, I have been able to work with outstanding colleagues.
"For example, that 'eye disease in a dish' investigation would not have been possible without the involvement of Dr. Janet Sparrow [Columbia, who received a 2007 RPB Senior Scientific Investigator Award for related research] whose process to age the stem cell-derived retinal cells we had created was fundamental to our success. Other labs had created retinal cells in the same manner but, like ours, they were immature and did not display mechanisms or characteristics of disease. Dr. Sparrow's aging process mimics some of the factors that promote the development of AMD.
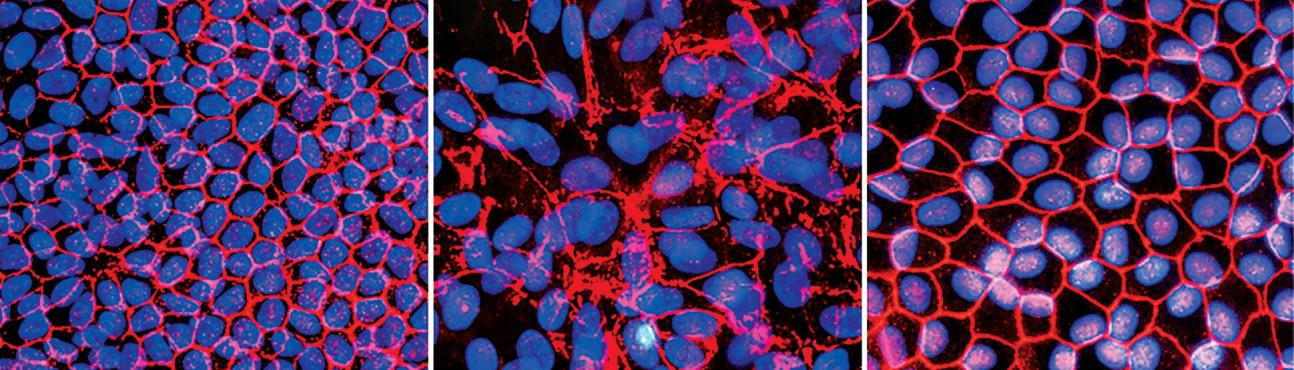
Images of a restored retinal structure from Dr. Tsang's research:stem cells from a normal individual (left) and from a patient with a form of retinitis pigmentosa (middle) were induced to become retinal pigment epithelial cells. The cells derived from the RP patient show abnormal protein (red) surrounding the cells (blue). This defect was corrected by gene therapy treatment (right), showing it is possible to correct a genetic defect in induced disease-state cells.This methodology provides a way to test patient-specific gene therapies in a dish.
"Vision scientists have arrived at a remarkable point in our journey to eventually prevent vision loss. We can now analyze an adult's genetic profile and determine with high accuracy whether he or she is at risk for developing retinal diseases. And we have demonstrated that we can use the patient's skin cells to grow retinal cells that will not be rejected by the patient's body.
Theoretically, with new and rapidly emerging techniques, we can remove defective genes and replace them with healthy genes as needed…and these rebuilt photoreceptors will integrate with the patient's visual circuitry.
"But before we get to actual tissue replacement, the first uses of these patient-specific retina cells will be for testing and refining of treatments. Instead of testing new drug candidates on thousands of patients, we will relatively quickly be able to screen for drugs on a couple of thousand cell lines.
"In fact, with flexible funds from my recent RPB Physician Scientist Award, I am conducting a high-risk, high-payoff project in this area that would not be supported by conventional federal granting mechanisms. So you see, with RPB support, one is able to lay the groundwork for a creative career as a researcher."
June 8, 2015
Subscribe
Get our email updates filled with the latest news from our researchers about preventing vision loss, treating eye disease and even restoring sight. Unsubscribe at any time. Under our privacy policy, we'll never share your contact information with a third party.
| General Info | Grants | News & Resources |