Short History of RPB
The deepest gratitude will never be expressed—nor can it be. It will be found in the eyes of those who live after us, who drink in the visual beauties of life without fearing the loss of that vision, and who may say to themselves in momentary acknowledgement of this magnificent gift, 'It is wonderful to see!'
Jules Stein, MD
Founder, Research to Prevent Blindness
Inspired by the vision of its founder, RPB has made a significant impact on the field of vision research. Here are just a few of its contributions throughout the years:
1960
RPB identifies barriers impeding U.S. eye research and develops a program to stimulate more intensive and extensive eye research across the country. RPB officials convince Congress to direct $1 million to blindness research – the first amount ever specifically allocated for this purpose.
1962
22 medical research institutions receive RPB unrestricted grant support, including New York University, which expedites the use of a laser to repair torn retinas.
1964
The first and only exhaustive study of eye research in the U.S., "Ophthalmic Research: U.S.A.," initiated and financed by RPB, is presented at a symposium of the American Academy of Ophthalmology and Otolaryngology.
1965
A 1965 RPB landmark public opinion poll finds that, with the exception of cancer, Americans fear blindness more than any other disease.
1966
RPB helps establish The Association of University Professors of Ophthalmology (AUPO) to evaluate and address problems facing the advancement of ophthalmic science in the nation's medical schools.
1967
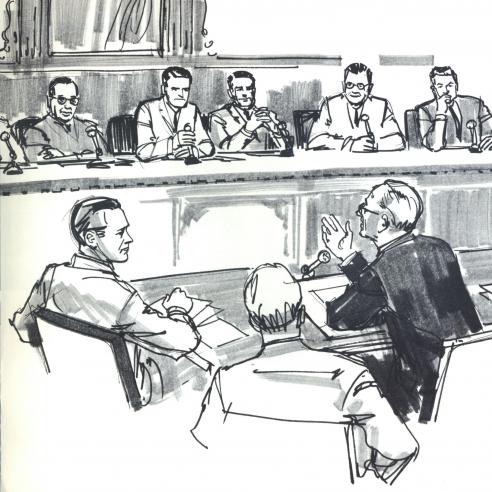 RPB Founder, Chairman and ophthalmologist Dr. Jules Stein testifies in favor of legislation to create a separate National Eye Institute (NEI).
RPB Founder, Chairman and ophthalmologist Dr. Jules Stein testifies in favor of legislation to create a separate National Eye Institute (NEI).
1968
Capping a five-year RPB initiative, President Lyndon B. Johnson signs legislation creating the National Eye Institute.
1970
The fundus camera, developed with RPB funds, enables stereo color photos of areas in back of the patient's eye during examination.
1974
 In ten years, RPB's Laboratory Construction Program more than triples the amount of eye research lab space in the U.S. With RPB support: vitrectomy, a new surgical procedure, is restoring sight to patients blind from diabetic hemorrhages; acute closed-angle glaucoma is cured by surgery; and corneas made of plastic are giving useful vision to hundreds of patients with otherwise untreatable corneal disease.
In ten years, RPB's Laboratory Construction Program more than triples the amount of eye research lab space in the U.S. With RPB support: vitrectomy, a new surgical procedure, is restoring sight to patients blind from diabetic hemorrhages; acute closed-angle glaucoma is cured by surgery; and corneas made of plastic are giving useful vision to hundreds of patients with otherwise untreatable corneal disease.
1979
RPB stimulates Congress to provide $3 million in Federal assistance to 67 eye departments planning extensive research lab development.
1980
RPB investigators identify factors that prevent abnormal blood vessel growth, opening a new area of research with potential to treat and prevent diabetic retinopathy and related disorders—a discovery which leads to today's anti-VEGF injections to treat wet macular degeneration.
1981
Two RPB grantees - Torsten Wiesel and David Hubel - are awarded the Nobel Prize in Physiology or Medicine for their discoveries concerning information processing in the visual system.
1982
RPB sponsors a training program at The Johns Hopkins School of Hygiene and Public Health for candidates from underdeveloped countries to learn to implement blindness prevention programs and clinical research activities.
A "living contact lens" – donor corneal tissue frozen and shaped to the needs of the patient – is developed to correct refractive errors that cannot be resolved by other means.
1986
An RPB researcher identifies a human cancer gene which protects against retinoblastoma, a blinding and often fatal childhood eye tumor, making prenatal diagnosis possible.
1987
Freezing abnormal blood vessels is the first successful therapy for retinopathy of prematurity.
A new drug for uveitis, cyclosporine A, decreases autoimmune inflammations of the inner eye and improves visual acuity of many patients.
1992
An RPB researcher studies gene expression in retinal degeneration. It is the first of four RPB awards she is to receive, all supporting work which, in 2007, results in the first use of gene therapy to restore sight in patients with retinitis pigmentosa.
1996
RPB researchers: improve extended-wear contact lenses to eliminate corneal infections; develop a new drug to lower eye pressure in glaucoma patients; link smoking to macular degeneration; and find that a single dose antibiotic treats trachoma, the leading infectious cause of blindness worldwide.
1998
RPB researchers develop a drug to arrest factors that prompt growth of unwanted blood vessels in macular degeneration and diabetic retinopathy.
1999
A laser and dye treatment known as photodynamic therapy is shown to stabilize vision of selected patients with the "wet" form of age-related macular degeneration. The FDA approves the first drug for this use the following year.
RPB supports development of wireless video glasses that transmit signals to a laser-powered microchip implanted in the retina which may someday give blind patients sight. The device, FDA-approved in 2014 and known as the Argus 2, is currently restoring sight to patients.
2001
RPB research teams at three universities collaborate on gene therapy that gives partial sight to three dogs born blind, heralding a new age in eye research.
2004
The first treatment to interrupt wet AMD, made possible by earlier, RPB-supported research, is approved by the FDA, bringing new hope to those already suffering from the disease. A second drug soon follows.
2005
RPB investigators develop a gene therapy for the inherited blind-deaf disease Usher1B, a major type of retinitis pigmentosa.
2006
An RPB researcher solves one of the great mysteries of ocular science: the mechanism that keeps the transparent tissue of the cornea free of blood vessels.
A new approach to retinoblastoma greatly reduces the size of tumors, allowing patients to save the affected eye, without the side effects of standard chemotherapy.
RPB scientists stop a world-wide epidemic of a rare, aggressive fungal corneal infection, fusarium keratitis, among people using a specific contact lens solution.
2007
Gene therapy restores vision in three young adults with Leber's congenital amaurosis, and cures color blindness.
RPB scientists chemically signal the eye's own resources to regenerate retina cells, without transplanting retinal tissue or stem cells
2008
An RPB Stein Professor develops a donor-derived stem cell treatment that restores clarity to diseased corneas--the first evidence that stem cells can remodel human tissue.
An RPB researcher develops a computer system that exercises the brain, restoring sight lost from stroke.
Researchers identify long-sought myopia genes and find that exposure to red light activates myopia's genetic mechanism.
2009
 RPB researchers report that glaucoma likely originates in the brain, a paradigm shift in understanding the disease that opens the door to neuroprotective therapies.
RPB researchers report that glaucoma likely originates in the brain, a paradigm shift in understanding the disease that opens the door to neuroprotective therapies.
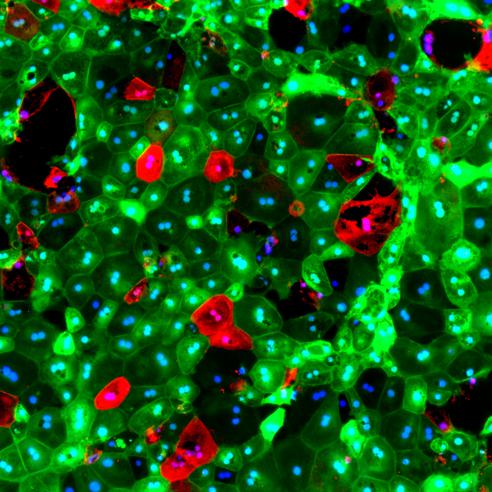
Researchers grow all seven classes of retinal cells using a new patient-specific stem cell made by inserting genes into skin fibroblasts, the most common type of connective tissue.
2010
RPB scientists create a nano knife, capable of surgically paring down nerve endings, demonstrating the possibility of creating a new family of micro-scale instrumentation that can extend surgical procedures down to individual cells and beyond.
RPB celebrates 50 years as the catalyst for vision research.
2011
As part of an effort to bring new technologies and cutting-edge translational science into ophthalmology, RPB launches the Innovative Ophthalmic Research Award to provide the means for departments of ophthalmology to develop collaborations with researchers working in other basic scientific disciplines.
A team of RPB researchers suggests that the recent, worldwide epidemic of myopia may be due to an imbalance in red-green cone stimulation caused by artificial lighting, computer monitors, tablet PCs and video games, particularly in genetically susceptible individuals.
A small clinical trial to test this concept reveals that using red-free glasses can slow the growth of the eye in children with early myopia.
2012
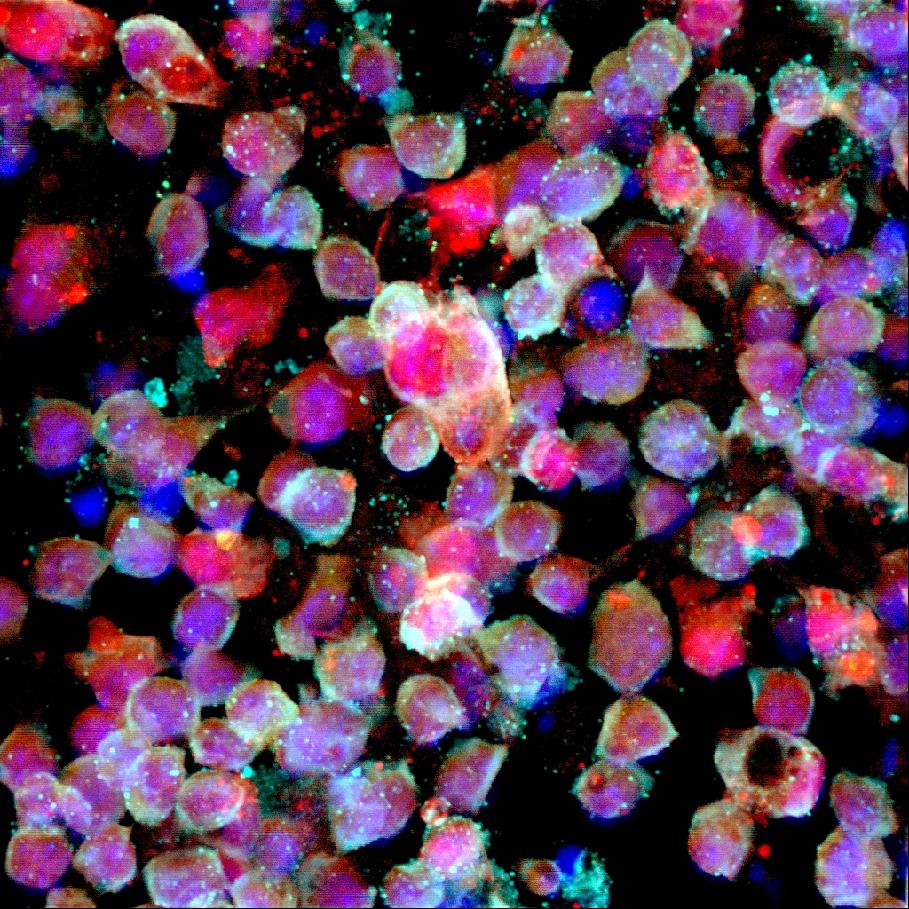
 RPB investigators announced a major advance in the field of vision restoration for patients with retinal degeneration: the creation of a chemical photo-switch that makes normally "blind" cells in the retina sensitive to light.
RPB investigators announced a major advance in the field of vision restoration for patients with retinal degeneration: the creation of a chemical photo-switch that makes normally "blind" cells in the retina sensitive to light.
A gene therapy for both the wet and dry forms of macular degeneration, developed by RPB researchers, enters human clinical trials.
2013
RPB conducts an internal strategic review of its grants programs, reinvents several of its major awards, and enters into innovative funding partnerships with other vision research-supporting organizations to create more impactful research support.
RPB scientists create bioengineered eye tissues, combining nano materials and stem cells. Next, they envision synthetic replacement tissue that can also deliver drug treatments when prompted by an eye drop "on-off switch."
2014
RPB hosts the first ever convening of vision research funders with the goals of identifying potential areas for collaborative action and stimulating partnerships throughout the vision research community.
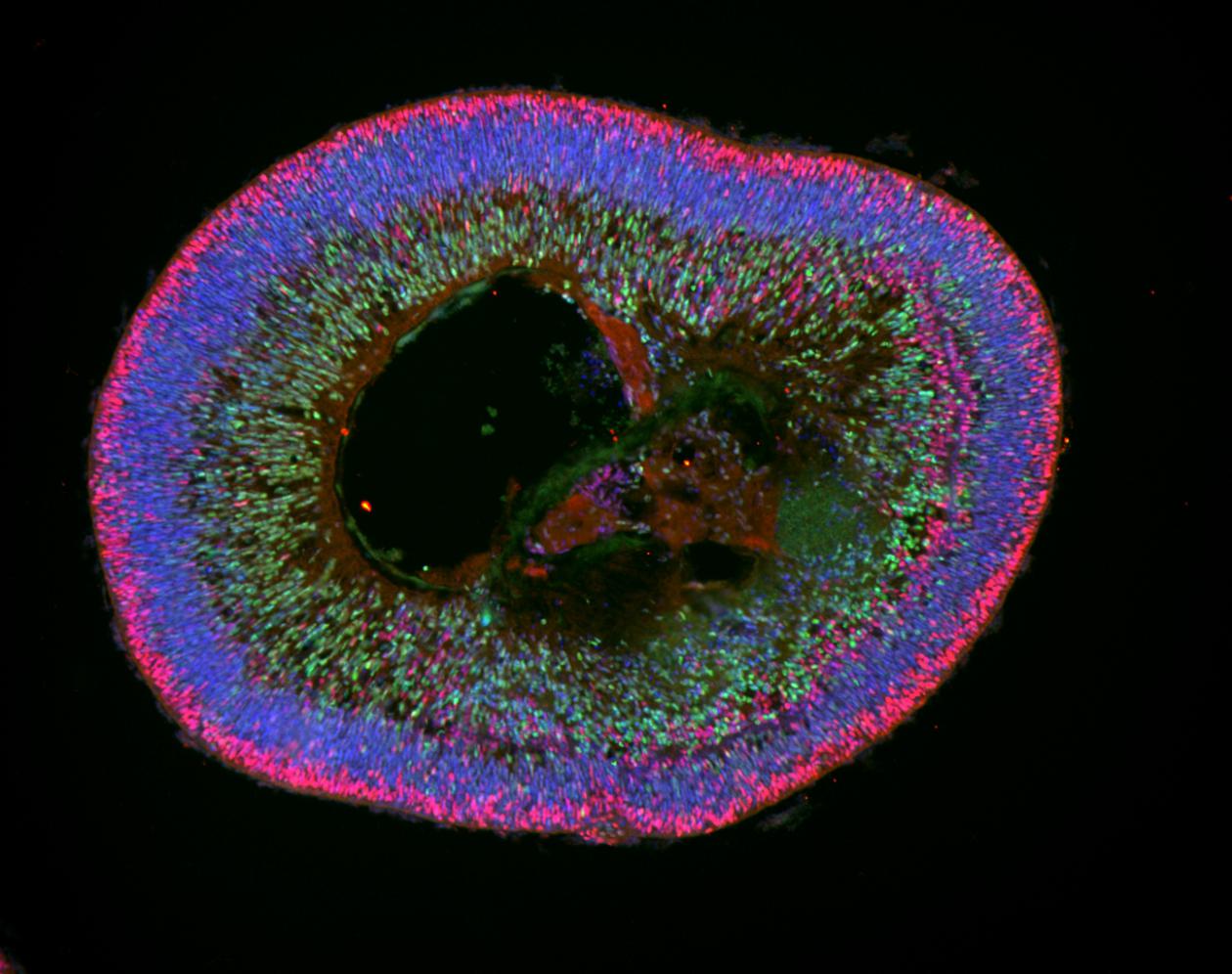
RPB-supported labs announce the development of light-sensitive retinas-in-a-dish, derived from patient skin and blood cells that can be used to test patient-specific treatments for retinal disorders.
2015
Months after he is deemed Ebola free, Dr. Ian Crozier, one of the earliest medical responders in the Ebola outbreak in West Africa, and an Ebola survivor, develops acute, sight-threatening eye inflammation. The Ebola virus is found living in his eye, posing a threat not only to Dr. Crozier and the ophthalmologists treating him, but to the 17,000 African Ebola survivors and the health workers treating them. Using flexible funds from RPB's Unrestricted Grant to the Emory Department of Ophthalmology, Steven Yeh, MD, successfully treats Dr. Crozier with corticosteroids and an experimental antiviral and develops a treatment protocol that is rolled out in Africa, saving the sight of thousands of Ebola survivors and preventing an Ebola resurgence from a previously unrecognized cause.
2016
RPB-supported researchers identify a potential treatment target for blinding diseases such retinitis pigmentosa and advanced dry age-related macular degeneration (AMD) by uncovering a pathway involved in the death of photoreceptors.
2017
RPB-supported researchers discover a biomarker that could help to predict glaucoma damage before vision loss.
2018
RPB-supported researchers and physicians administer the first FDA-approve gene therapy for inherited blindness; in just weeks, the patient (a 13-year-old boy), had significant improvements in his vision.
2019
RPB grantee Gregg Semenza, MD, PhD, is awarded the Nobel Prize in Medicine or Physiology for discoveries of how cells sense and adapt to oxygen availability; his RPB grant enables him to apply his Nobel-caliber knowledge and skills to vision research.
Subscribe
Get our email updates filled with the latest news from our researchers about preventing vision loss, treating eye disease and even restoring sight. Unsubscribe at any time. Under our privacy policy, we'll never share your contact information with a third party.
| General Info | Grants | News & Resources |